Dolly Parton was probably thinking about a love affair, not acid reflux, when she wrote: “Here You Come Again.” But if you’ve ever felt a meal starting to creep back up your throat, you could be forgiven for adopting the song as a lament about digestion gone wrong.
Acid reflux and its main symptom, heartburn, are uncomfortable and often painful conditions. And like many an ill-fated relationship, they’re fairly common — though they don’t get nearly as much attention in popular music.
Acid reflux may affect up to 1 in 5 people in industrialized countries. It’s widespread in the US, where as many as 1 in 3 people experience it at least once a week.
Acid reflux is often treated with medications, which come in both over-the-counter and prescription formulations. And while these medications can provide temporary relief, they don’t address the root cause of the condition. And they often come with significant side effects, especially when used over time.
So if Alka-Seltzer, Maalox, and Tums — and prescription histamine blockers and proton pump inhibitors (more on these below) — don’t resolve the underlying issues, what does? And what exactly causes acid reflux?
It turns out that diet is a known influence here — capable of both causing the problem and making the symptoms worse. So what’s the link between diet and acid reflux? And what foods should you be eating and steering clear of to avoid that “here it comes again” feeling?
What Is Acid Reflux?
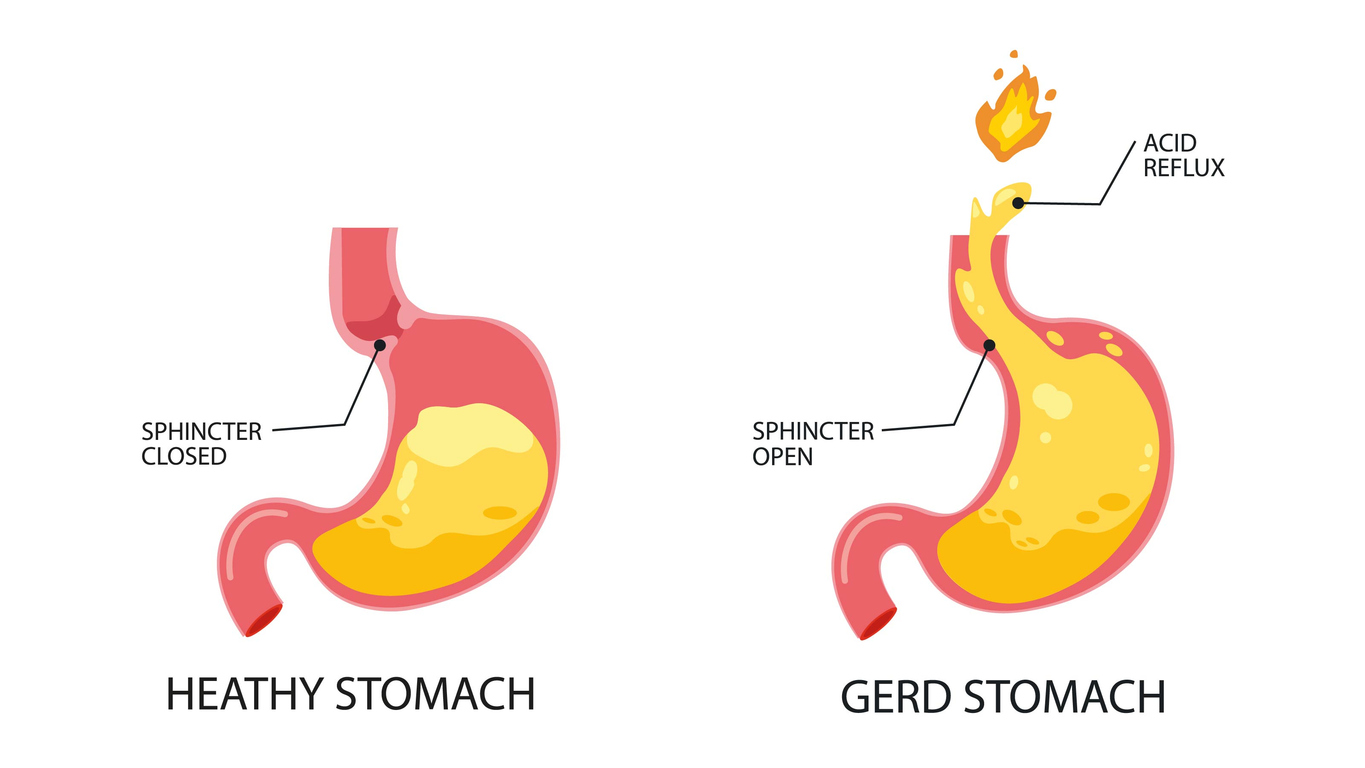
Before we talk about treatment and prevention, what exactly is acid reflux? Technically, it’s when stomach acid flows back into your esophagus (the tube that connects your mouth to your stomach). This is a problem because, unlike your stomach, your esophagus isn’t set up to handle extremely acidic substances. And when food reaches your stomach, it gets mixed with highly acidic gastric juices. So that bolus of food and gastric juices going the wrong way can irritate the lining of your esophagus.
Symptoms of acid reflux irritation can include a burning sensation in your chest (heartburn), regurgitation of food or sour liquid, and difficulty swallowing.
When the condition becomes chronic and more severe over time, it’s known as GERD or gastroesophageal reflux disease. A recent study indicates a potential link between GERD and increased cardiovascular risk factors, including elevated blood pressure and unfavorable lipid profiles. This association underscores the importance of comprehensive management of GERD to mitigate potential systemic health risks.
Most people can manage the occasional case of acid reflux with lifestyle changes and over-the-counter medications. In contrast, GERD flare-ups can be frequent and severe enough to require a more intensive medical intervention.
There are a few different types of GERD, each of which probably deserves its own country song. There’s the provocatively named NERD (non-erosive reflux disease), the most common type, which is characterized by reflux that hasn’t yet damaged the mucosal lining of the esophagus.
By contrast, in ERD (erosive reflux disease), the acidic contents of the stomach have eroded at least some of the esophageal lining.
LPR, or laryngopharyngeal reflux, happens when the acidic mixture makes it all the way into the throat, where it can wreak havoc on the glottis and vocal cords. Symptoms include hoarseness, chronic throat clearing, and “globus sensation,” or, as it’s more commonly known, having a lump in the throat.
The last kind I’ll mention is Barrett’s esophagus (BE). In BE, the body performs a clever adaptive trick: It replaces the sensitive esophageal lining with tissue that’s very similar to the lining of the intestines — that is, tissue that’s able to handle the acid reflux without erosion.
The problem is, BE is often a precursor to esophageal adenocarcinoma, a type of cancer of the esophagus that can be difficult to detect until late stages. And at that point, there’s not a lot that can be done about it.
How Are Acid Reflux and GERD Commonly Treated?
Drugs are the medical mainstream’s most commonly advised and prescribed treatments for acid reflux and GERD, even though there’s evidence that dietary and lifestyle adjustments can help manage both conditions (more on this below).
If you’re in the habit of watching pharmaceutical ads for heartburn on television, you may notice that one of the most common themes is, “If you take this drug, you can keep eating the stuff that’s been causing the problems.” But as you’ll see, that might not be the best long-term solution.
Over-the-Counter (OTC) Drugs

Antacids are the main OTC treatment for heartburn and acid reflux. And they provide temporary relief. But in some cases, over time, they can have some serious downsides. In 2022, the US Food and Drug Administration (FDA) published a warning that antacids that contain aspirin can cause stomach and intestinal bleeding.
Common side effects of the main kind of antacid, those containing calcium carbonate (like Tums), include abdominal pain, constipation, nausea, vomiting, and flatulence — as well as a nasty turn of events known as “acid rebound.” This is when the stomach notices that its acid levels have dropped, and ramps up the production of acid to compensate.
There’s evidence that taking antacids for a long time can compromise your heart health, too. The main component of many antacids, calcium carbonate, can bring excess calcium into the bloodstream and lead to the formation of plaque. One study found that adults who use antacids are more likely to experience a heart attack than people who don’t use antacid drugs.
Prescription Medications for Acid Reflux and GERD
The two commonly prescribed classes of medication for reflux and GERD are histamine type 2 (H2) receptor blockers and proton pump inhibitors (PPIs).
They’re more powerful than the OTC formulations, which unfortunately increases the likelihood and severity of unwanted side effects. A 2021 review of the scientific literature offered this laundry list of risks: “… kidney, liver, and cardiovascular disease, dementia, enteroendocrine tumors of the gastrointestinal tract, susceptibility to respiratory and gastrointestinal infections, and impaired absorption of nutrients.” And a 2024 study found long-term use of PPIs has been associated with decreased bone mineral density and an increased risk of fractures, particularly in men.
But wait, there’s more!
By lowering stomach acid, PPIs can compromise gut health and actually increase the risk of foodborne infections. That’s because one of the body’s lines of defense against pathogens in food is a highly acidic digestive system. And reducing acid production can create an environment where nasty little critters can thrive and reproduce. They can also make the body more susceptible to airborne diseases such as pneumonia.
But wait, there’s even more! (This is starting to feel like the world’s worst infomercial!) A 2024 study found an association between antacids, migraines, and severe headaches. These included both OTC and prescription formulations: Prilosec, Prevacid, Nexium, Pepcid AC, Zantac 360, Tums, and Alka-Seltzer.
Vonoprazen, a new medication, is a potassium-competitive acid blocker (PCAB), which claims to offer faster and longer-lasting relief for GERD symptoms compared to traditional proton pump inhibitors (PPIs). However, long-term use of vonoprazan (over a year) may increase the risk of developing stomach growths called fundic gland polyps.
The acid reflux drugs can also become less effective in managing symptoms over time, at which point medical professionals may recommend stronger medication or even surgery for GERD.
The Link Between Diet and Acid Reflux

The trouble with most acid reflux medications is that they focus on making the stomach environment less acidic. This can help with short-term symptoms — but as we’ve seen, over time, it can also cause problems.
While stomach acid can be excessive, the core problem that causes acid reflux, heartburn, and GERD is when the stomach’s natural acidity backwashes into the esophagus.
So what causes partially digested food and gastric juices to go in the wrong direction?
In general, relaxation is good, but there are some exceptions. One of those exceptions applies to a muscle called LES, the lower esophageal sphincter. Sphincters are one-way valves, or at least they’re supposed to be. And your LES is there to prevent the contents of your stomach from refluxing back up into the esophagus.
If the LES gets too relaxed, it can’t do its job, and acid reflux can result. Certain foods are frequent culprits that tend to over-relax the LES. These include alcohol, fatty foods, and chocolate.
There’s also an LES dysfunction caused by an overly distended stomach. When stretched too much by food or even air (from carbonated beverages, for example), the LES can spontaneously relax, and that one-way street can become a very chaotic two-way boulevard.
The triple threat for esophageal acid exposure is a meal high in calories, high in fat, and high in volume. And certain foods are more likely to cause excess stomach acid secretion in susceptible people. These can include “spicy food, citrus fruits, tomatoes, onions, garlic, chocolate, mint, caffeinated beverages, alcohol, and carbonated drinks,” according to one scientific article on GERD. Timing matters as well — eating close to bedtime can also contribute to acid oversecretion.
On a population level, unhealthy dietary patterns high in fat, sugar, salt, and cholesterol are contributing to the increasing incidence of chronic diseases like GERD.
What to Avoid with Acid Reflux
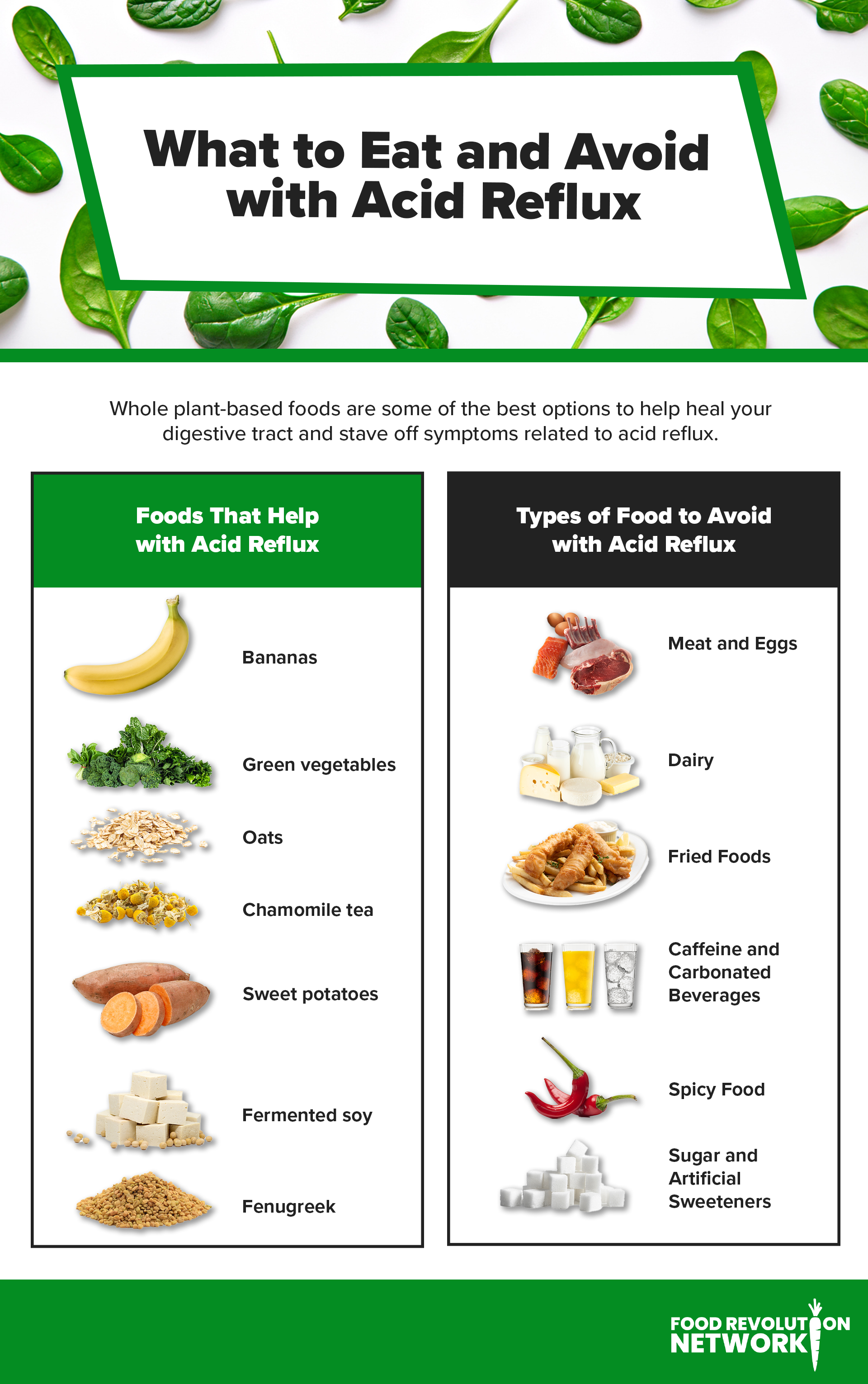
If you suffer from acid reflux, a good place to start addressing it is to reduce your sugar and fat intake. Here are some specific classes of foods that you may want to decrease or eliminate:
Meat and Eggs

A study from Ireland found that people who consumed the most red meat, processed meat, and saturated fat had the highest rates of acid reflux. The top fifth of red meat eaters had roughly three times the risk of esophageal adenocarcinoma (the type of cancer mentioned earlier).
A survey of over 1,000 Italians found that vegans were half as likely to experience GERD as non-vegans. Non-vegan foods such as meat, fish, poultry, and eggs all contributed to the difference in outcomes.
Other research also points to foods of animal origin as being particularly problematic. A 2021 review of the scientific literature on food and GERD found that vegetarian diets produced less GERD, while consumption of meat, eggs, and fish increased the risk.
Fatty and Fried Foods
Fat contributes to acid reflux because it slows down the emptying of the stomach, which can cause stomach acid to build up and back up into the esophagus. Additionally, fatty foods can relax the lower esophageal sphincter, making it easier for acid to escape from the stomach. Given that they’re high in fat, it’s no surprise that fried foods tend to be among the worst offenders. This has been shown to be true in a variety of regions, including Korea, Saudi Arabia, and the US.
Sugar and Artificial Sweeteners

A 2021 study found that “free sugar” consumption among Chinese adolescents predicted laryngopharyngeal reflux (LPR), with the highest sugar consumers 65% more likely to experience reflux.
Other studies suggest that all sugars, including artificial ones, are associated with reflux and GERD. A 2017 study found a correlation between sugar consumption and BE, with those eating the most sugar at 70–80% higher risk of the disease.
Caffeine and Carbonated Beverages
The huge Nurses’ Health Study II has followed the health and diets of almost 50,000 US nurses for an average of over 5 years. In 2020, researchers published findings that coffee, tea, and fizzy drinks were associated with a roughly 30% increased risk of GERD.
For coffee and tea, statistical analysis suggested that it was specifically the caffeine in these beverages that was associated with reflux. The carbonated beverage mechanism was the phenomenon we saw earlier. The gasses in those drinks can reduce LES pressure and increase relaxation, which can allow highly acidic stomach contents to bubble back up into the esophagus. Of course, if carbonated beverages are sugary soft drinks, then that might make them something of a twofer, but in a very unpleasant way.
If you have reflux issues and can’t bear the thought of giving up your morning (or noon, afternoon, or evening) cup of joe, some studies have found that dewaxed coffee produces less heartburn than waxed coffee.
When I looked up the difference between waxed and dewaxed coffee, I found, to my relief, that it had nothing to do with leg hair removal. Instead, dewaxing is a process that removes the coffee bean’s waxy outer layer, which many people find difficult to digest anyway.
Although dewaxed coffee is considered low-acid, all low-acid coffee is not dewaxed. Look for brands that say dewaxed on the label or “caffe decerato” on Italian coffee brands. Two brands that sell dewaxed coffee are Lavazza and Carraro.
Spicy Food

If there’s a poster child for heartburn, it’s the “spicy food” group. And while many spices can deliver significant health benefits, it could be that people who frequently suffer from heartburn should consider keeping their spice levels low.
Capsaicin is a chemical compound that makes food taste spicy. It appears that it also activates TRPV1 receptors in the esophagus, producing a burning sensation.
A small Mexican study looked at what happened when 31 people who’d been diagnosed with GERD were given capsaicin; 28 of them reported symptoms such as heartburn and chest pain.
A 2020 study from Iran found that men who ate lots of spicy food (“lots” defined as 10 or more times per week) had about 2.5 times the heartburn compared to men who avoided spicy foods. Interestingly, no such pattern emerged in women.
Can a Plant-Based Diet Help?

Given that many processed and animal-sourced foods appear to worsen GERD, you might expect that reducing or eliminating them would make things better. And that’s exactly what some research shows.
Two 2023 studies from Italy, each surveying over 1,000 adults, found that vegans had roughly half the rate of GERD as non-vegans. These studies are particularly noteworthy because the researchers went out of their way to include lots of vegans — over 400 of them, actually — which gave them enough statistical power to find meaningful differences between vegans and non-vegans.
The differences between animal and vegetable protein may explain at least some of these findings. A 2018 study looked at how the bodies of people with heartburn reacted differently to meals containing animal versus vegetable protein in the hour after consumption. They had less reflux and less esophageal exposure to stomach acid following the vegetable protein meal compared to the animal protein one.
There’s a lot of evidence that it’s not just what you don’t eat that can make a difference in reflux frequency and severity; foods sourced from plants that are unprocessed or lightly processed have been shown to both prevent GERD and reduce symptom production.
A 2017 study of almost 4,000 adults showed that people who ate the most fruits and vegetables had a 33% lower risk of developing GERD than those who ate the fewest.
One of the things in fruits and vegetables that helps with reflux and GERD is fiber. A diet rich in fiber has been shown to increase LES resting pressure, reduce the amount of reflux, and decrease the incidence of heartburn.
Fiber also has a positive impact on the gut microbiome. This is important because damage to the microbiome may be one of the causes of reflux.
Key Plant-Powered Foods and Drinks That May Help with Acid Reflux

Bananas
Bananas can help reduce reflux through their ability to neutralize stomach acid.
Green Vegetables
Green vegetables have been shown to reduce reflux during pregnancy.
Oats
Oats have lots of fiber, which we’ve seen helps reduce heartburn. And oatmeal can have a soothing effect on the lining of your stomach.
Chamomile Tea
Chamomile tea is also calming to the digestive system, as well as anti-inflammatory.
Sweet Potatoes
Sweet potatoes have been used for centuries to relieve digestive ailments. A 2021 study found that drinking sweet potato juice significantly reduced heartburn, as well as the unpleasant sensations behind the breastbone that can be caused by GERD.
Fermented Soy
Fermented soy products may decrease reflux. A 2020 study found that fermented soy supplements may reduce the frequency of heartburn over time. And if you prefer actual food to supplements, miso soup is a form of fermented soy that has, specifically, also been shown to lessen GERD symptoms.
Fenugreek
Fenugreek is another traditional digestive remedy that’s been shown to decrease heartburn frequency and severity.
Other Lifestyle Changes to Consider
In addition to the dietary approach, several lifestyle upgrades can help prevent and manage reflux and GERD.
People who are obese are at increased risk of GERD. In addition to eating more plant-based foods and fewer foods of animal origin, weight management strategies can include avoiding soft drinks, fast foods, and large portions.
Stress can also contribute to GERD, so stress management strategies can help prevent or reduce incidents of reflux.
Quitting smoking can also help, as smokers tend to have chronically low pressure in their LES, and reflux events increase during periods of smoking. A 2023 study found that the risk of reflux esophagitis is roughly 2.5 times greater for current smokers than nonsmokers.
Drinking alcohol can damage the mucous membranes of the esophagus and increase symptoms of GERD. A 2022 study found that alcohol consumption of more than 70 grams a week for men and more than 140 grams a week for women increased the risk of developing erosive esophagitis.
In addition to what you eat, how and when you eat can also affect reflux symptoms. Eating and drinking between meals and eating close to bedtime are both associated with more GERD.
One more tip: You can reduce the occurrence of GERD and improve digestion by utilizing the “left lateral decubitus” sleeping position. Translation: Sleep on your left side with your legs slightly curled. And resist the urge to lie down right after eating.
Recipes to Help Combat Acid Reflux
Discover the healing powers of plants with these simple and tasty plant-based recipes crafted to help alleviate acid reflux. Each dish offers ingredients that are gentle on the digestive system. From hearty vegetable bowls to soothing tea, these recipes are not only designed to ease symptoms but delight the palate. Whether you’re seeking a nourishing breakfast, a light lunch, or a comforting dinner, these meals offer delicious and effective solutions for maintaining digestive health naturally and enjoyably.
1. Soothing Chamomile Ginger Tea

Soothe your stomach with a cup of Chamomile Ginger Tea, a calming and aromatic blend that aids in managing acid reflux. This tea combines chamomile, known for its soothing properties on the digestive system, with ginger, which helps reduce inflammation and promote digestion. Dried fennel seeds are added to reduce stomach acidity and improve overall digestive health, while a hint of lemon not only enhances the flavor but also provides vitamin C and antioxidants. Enjoy this tea after meals or whenever you need relief from digestive discomfort — it’s a natural and gentle solution to support a happy tummy.
2. Baked Carrot Cake Oatmeal
 Baked Carrot Cake Oatmeal is a comforting and nutritious breakfast that may help ease acid reflux symptoms. A delicious blend of organic rolled oats and buckwheat flour with anti-inflammatory spices like cinnamon, ginger, and turmeric helps soothe the digestive system. Chia seeds and walnuts add healthy fats and fiber for improved digestion, while carrots provide natural sweetness and extra fiber. The use of plant-based milk and yogurt creates a creamy texture without the acidity of dairy, ideal for those with acid reflux. Sweetened lightly with maple syrup and vanilla extract, this oatmeal is a delicious and gentle way to start your day.
Baked Carrot Cake Oatmeal is a comforting and nutritious breakfast that may help ease acid reflux symptoms. A delicious blend of organic rolled oats and buckwheat flour with anti-inflammatory spices like cinnamon, ginger, and turmeric helps soothe the digestive system. Chia seeds and walnuts add healthy fats and fiber for improved digestion, while carrots provide natural sweetness and extra fiber. The use of plant-based milk and yogurt creates a creamy texture without the acidity of dairy, ideal for those with acid reflux. Sweetened lightly with maple syrup and vanilla extract, this oatmeal is a delicious and gentle way to start your day.
3. Sweet Potato Lentil Bowl with Green Tahini Sauce

Dive into this Sweet Potato Lentil Bowl topped with Green Tahini Sauce, a comforting meal perfect for those looking to ease digestion and manage acid reflux. The hearty lentils and sweet potatoes not only fill you up but also help neutralize stomach acid thanks to their fiber content and alkaline nature. Packed with vegetables like spinach, beets, and carrots, this bowl is loaded with nutrients that promote good digestion. The creamy Green Tahini Sauce adds a delicious richness without heavy fats, making it gentle on your stomach. Sprinkled with aromatic Dukkah Seasoning for a bit of crunch, this bowl is as tasty as it is beneficial for your digestive health.
Attention to Diet and Lifestyle Is Essential for Acid Reflux
Acid reflux and GERD are common and often uncomfortable. Medical interventions are sometimes helpful but may come with dangerous side effects. Fortunately, dietary adjustments and lifestyle changes can help, and may even prevent or reverse these conditions.
Certain foods and eating habits play a crucial role in exacerbating or alleviating the symptoms of acid reflux. Incorporating more plant-based foods and reducing triggers such as fatty meats, caffeine, and spicy foods can significantly mitigate symptoms and improve quality of life. Lifestyle adjustments such as quitting smoking, reducing alcohol consumption, and optimizing meal timing and sleep posture can further improve your digestive health.
Ultimately, understanding and adapting your diet and lifestyle in response to acid reflux and GERD may not only alleviate symptoms but also contribute to a healthier, more vibrant life.
Tell us in the comments:
- What will you change about your diet now that you know its impact on acid reflux?
Featured Image: iStock.com/Tharakorn



