Philosopher and psychologist William James is quoted as saying, “Is life worth living? It depends upon the liver.”
I’m guessing he was referring to the person living that life — their goals, passions, circumstances, predispositions, those sorts of things.
But you might also take his response literally. Your very existence depends upon the liver in your body: the heaviest organ you’ve got and, arguably, the one doing the most complex tasks to keep you alive.
It’s been described as a manufacturing hub, a processing plant, and a storage facility. Without your liver, you couldn’t digest food, build new tissues, remove toxins, or store useful nutrients to be used later.
That’s reason enough to pay attention to a condition called NAFLD, which is not a new football league but rather the acronym for nonalcoholic fatty liver disease. NAFLD, though not as well-known as diabetes, heart disease, or cancer, is nevertheless incredibly widespread.
Also known as metabolic dysfunction-associated steatotic liver disease, or MASLD, it’s the leading cause of liver disease worldwide, affecting at least a quarter of the world’s adult population. More than 75% of people with obesity and up to 90% of those with severe obesity also have NAFLD.
It’s an expensive condition, too — health economists estimate the annual direct cost of NAFLD in the United States alone to be over $100 billion (yes, with a “B”) — even though it’s largely undiagnosed. That’s because it’s so prevalent and, in its serious later stages, requires expensive, multidisciplinary care.
Early stages of NAFLD are asymptomatic, so it’s common for people not to catch the condition early enough to treat it effectively. By the time it’s diagnosed, it’s often accompanied by complications that current medical standards of care cannot reverse. Alarmingly, having NAFLD increases your risk of dying in the next 15 years by 34–69%.
Noting that the rising prevalence of NAFLD closely tracks the twin epidemics of obesity and type 2 diabetes, some health researchers point out that it may share root causes with those and other metabolic diseases.
So, what causes NAFLD? How do you know if you have it? And can diet and lifestyle help prevent or reverse it?
What Is Nonalcoholic Fatty Liver Disease (NAFLD)?
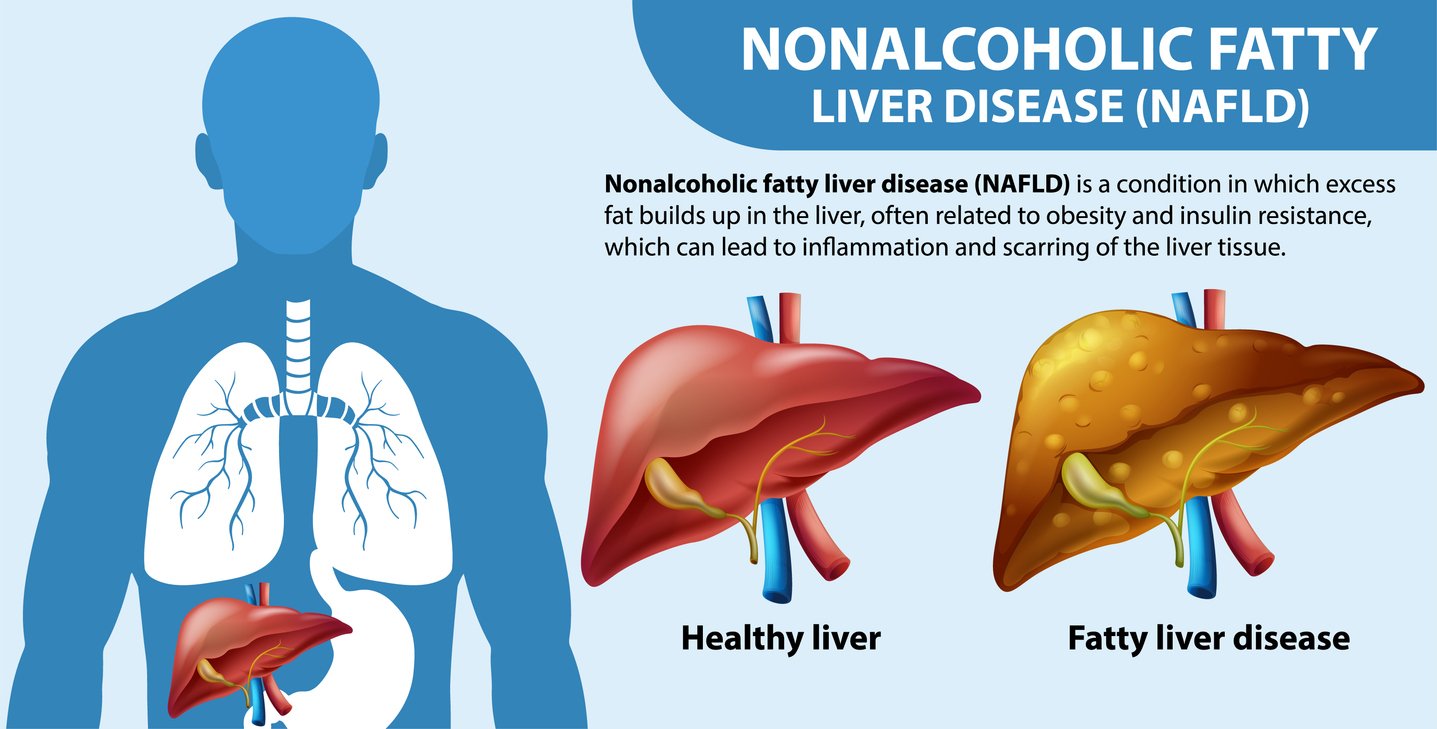
NAFLD is a spectrum of liver diseases, ranging from an initial buildup of fat in the liver (called steatosis) to dangerous and nonreversible scarring (aka cirrhosis).
NAFLD typically progresses slowly, with each stage of fibrosis (scarring) lasting about seven years. Simple fatty liver, the earliest stage, consists of fat buildup without inflammation. Eventually, it may progress to liver damage via a condition called nonalcoholic steatohepatitis (NASH), and ultimately, cirrhosis (nonreversible scarring and damage) and even liver cancer.
NAFLD is differentiated from the kind of liver disease that can be caused by excess alcohol consumption. It’s associated not with drinking but rather with metabolic syndrome. NAFLD typically results from an accumulation of excess free fatty acids and triglycerides. Other factors that can fuel it can include some medications, hormonal disturbances such as hypothyroidism, and nutritional imbalances.
NAFLD Symptoms
One of the most dangerous things about NAFLD is that most people don’t experience any symptoms in the early stages of the disease when they might be able to do something about it before it causes permanent damage.
If NAFLD progresses to the NASH stage, symptoms often include fatigue, unexplained weight loss, weakness, and, most specifically, a dull pain or ache in the top right of the stomach, under the ribs (known to medical professionals as the RUQ, or right upper quadrant of the abdomen, home to the liver, gallbladder, pancreas, and sections of the small intestines).
If NAFLD further progresses to cirrhosis, it can lead to jaundice and edema.
Fatty Liver Disease Screenings

There are a few potential diagnostic tests that can help discover NAFLD. Before we get into them, it’s important to note that most medical associations do not recommend using them to screen the general population. That’s because insurance companies have not deemed screening cost-effective.
Insurance companies don’t think NAFLD screening is cost-effective in most cases because of the widespread belief that there aren’t any useful therapies for it. While that’s true in the narrow sense that there aren’t many billable medical interventions that can slow, halt, or reverse the condition, as we’ll see below, there are powerful lifestyle strategies that can drastically change the disease’s trajectory in many, if not most, cases.
Diagnostics in High-Risk Patients
International medical associations recommend NAFLD evaluation in high-risk patients. These include people with type 2 diabetes or prediabetes, elevated levels of an enzyme produced by the liver called serum alanine aminotransferase (ALT), or the presence of fatty liver on imaging studies.
So, how is NAFLD diagnosed? Unfortunately, the least invasive options, such as a liver function test or ultrasound, are the least reliable. The gold standard method of assessment, liver biopsy, has a few downsides: high cost, potential sampling error (since fatty deposits are unevenly distributed in the liver, the results could be skewed based on where the sample was taken), and complications such as bleeding, infection, and pain (although the risks of these complications are low).
Other newer diagnostic methods are noninvasive and are often used to monitor the presence and progression of NAFLD in high-risk patients. Some of these tests are called (get ready for some “acronym soup” here) FIB-4, NFS, ELF, VCTE, and MRE.
What Causes NAFLD?

NAFLD has its roots in genetic, environmental, and lifestyle factors. Genetic predispositions to the disease can be either conferred at birth or due to gene mutation. Environmental triggers for the development and progression of NAFLD include chemicals like inorganic arsenic and plastics like vinyl chloride.
But the biggest factor is lifestyle — especially diet.
NAFLD typically accompanies other conditions related specifically to poor diet. As we’ve seen, most obese adults also have NAFLD, and 90% or more of people with hyperlipidemia (high cholesterol levels) have it, too.
One of the major mechanisms of NAFLD is insulin resistance. That’s because insulin acts as a shuttle to get carbohydrates into cells so they can use them as energy. When the body struggles with this process, those carbohydrates have no place else to go, and they can end up turning into fatty deposits in the liver.
Other people at risk for developing nonalcoholic fatty liver include those with polycystic ovary syndrome, underactive thyroid, high blood pressure, chronic kidney disease, obstructive sleep apnea, or people who smoke. These conditions are all largely associated with low-quality diets.
The Worst and Best Foods for NAFLD
If NAFLD is largely caused and worsened by diet, what are the foods to avoid and the ones to double down on?
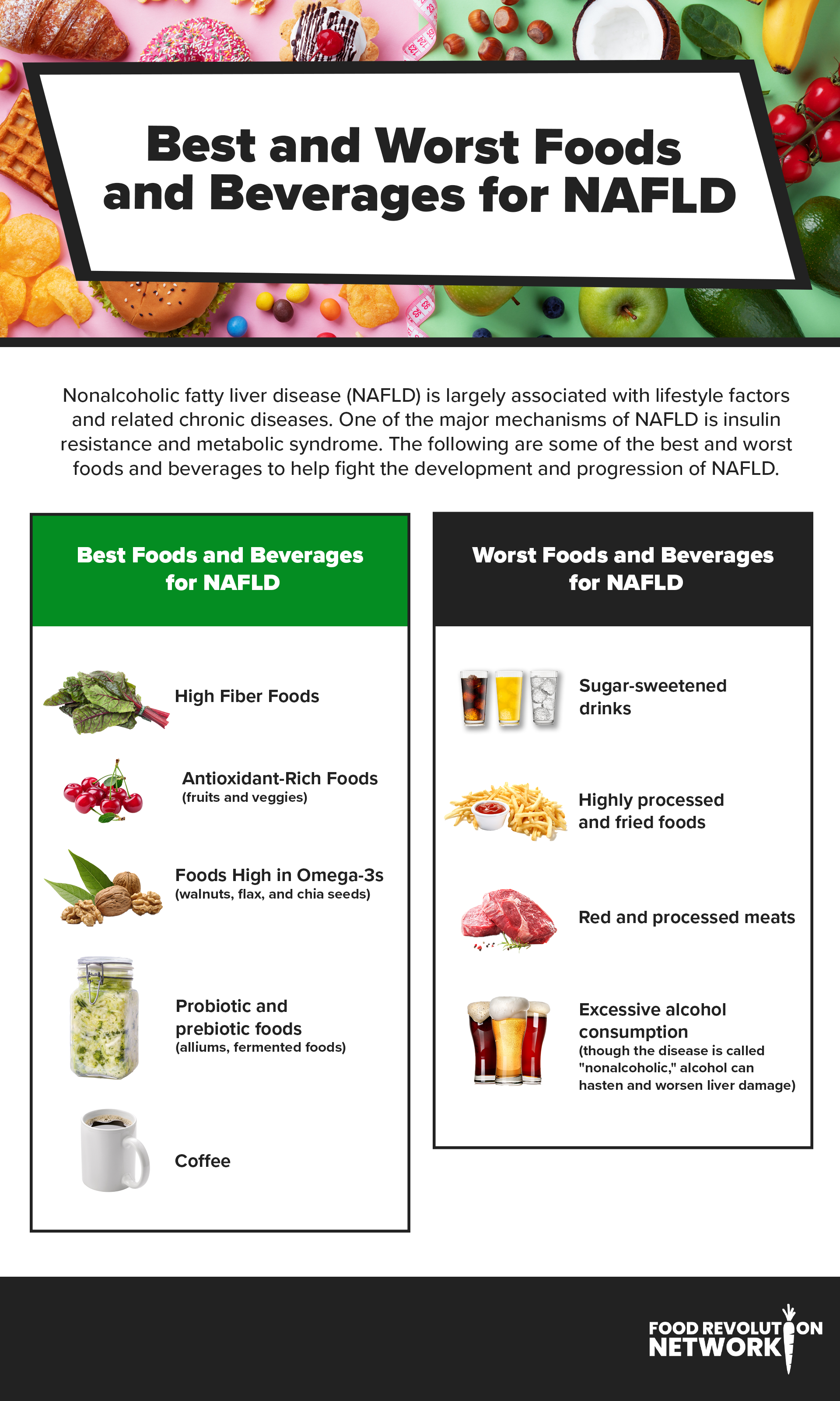
The worst foods for NAFLD include the following:
- Sugar-sweetened drinks (soda, fruit juices, etc.)
- Refined carbs (white bread, pastries, etc.)
- Highly processed and fried foods (chips, fast food, etc.)
- Red and processed meats (bacon, sausages, etc.)
- Excessive alcohol consumption (though the disease is called “nonalcoholic,” alcohol can hasten and worsen liver damage)
Of these, red meat and sugar-sweetened beverages have been shown to have the strongest association with NAFLD symptoms and progression.
The best foods for NAFLD are those that fight heart disease and metabolic issues, such as:
- Minimally processed plant-based foods rich in fiber, such as whole grains, fruits, and vegetables
- Antioxidant-rich foods and beverages (berries, nuts, leafy greens, green tea — and especially those that are good sources of Vitamin E)
- Food rich in omega-3 fatty acids, including plant-based sources like flaxseeds, chia seeds, walnuts, and hemp nuts
- Probiotic and prebiotic foods (kimchi, sauerkraut, garlic, onions) to improve gut health
- Coffee (which may help reduce liver inflammation)
Can You Reverse Nonalcoholic Fatty Liver Disease?

Once you’ve got it, is the best you can hope for to manage NAFLD? Or is it possible to reverse the process and remove fatty deposits from your liver?
Several studies have shown that it’s possible to shed liver fat. The most powerful tool is probably changing your diet and swapping out animal products and highly processed junk food for whole, plant-based foods. Many experts recommend a Mediterranean-type dietary pattern. (Check out our advice on how to implement a Mediterranean plant-based diet.)
Exercising can help, too. Aim for at least 150 minutes of moderate activity per week for maximum benefit.
Both strategies can support weight loss, a powerful way to reduce liver fat. Studies show that for people with excess fat, losing 7–10% of body weight can significantly reduce liver fat.
Improving gut health can also help. Both increasing fiber intake and adding prebiotics and probiotics can address NAFLD by building up populations of beneficial bacteria that can mitigate insulin resistance.
In terms of medical treatments and interventions that target liver fat as a pathway to NAFLD and its progression into NASH and cirrhosis, there’s ongoing research. Still, no specific drugs are on the market at this time.
That’s why it’s so important to manage underlying conditions like type 2 diabetes, high blood pressure, excess weight, and high cholesterol as a means of preventing, slowing, or even potentially reversing NAFLD.
Recipes for Liver Health
Nourish your body and support liver health with these three vibrant, plant-based recipes! From the refreshing Fennel, Orange, and Avocado Salad to the cozy warmth of Soothing Spiced Matcha, each recipe is packed with ingredients known for their detoxifying and anti-inflammatory benefits. Whether you’re in the mood for a crisp salad, a creamy matcha drink, or something in between, these dishes make it easy — and delicious — to give your liver some TLC!
1. No-Cook Yogurt Oats

This No-Cook Yogurt Oats is a quick, nutrient-rich breakfast that’s great for liver health! Creamy plant-based yogurt and oats pack in fiber and probiotics, while date paste brings natural sweetness without refined sugar. Walnuts and flaxseeds add anti-inflammatory omega-3s, and the antioxidant-rich blueberries and coconut support liver detoxification. Mix it up, chill, and wake up to a breakfast that’s as delicious as it is nourishing!
2. Fennel, Orange, and Avocado Salad

This Fennel, Orange, and Avocado Salad is a refreshing, zesty boost for your liver health! Crisp fennel, juicy oranges, and creamy avocado come together on a bed of kale, bringing fiber, vitamin C, and healthy fats that aid liver function and support detoxification. Tossed with a tangy Orange Miso Dressing packed with probiotics and anti-inflammatory ginger and topped with cranberries, almond slivers, and green onion, it’s as tasty as it is nourishing!
3. Soothing Spiced Matcha Tea

This Soothing Spiced Matcha Tea is the perfect blend of warmth and vitality, giving your liver extra love with each sip! Antioxidant-rich matcha supports detox, while turmeric, cinnamon, and nutmeg add anti-inflammatory warmth. Black pepper boosts the turmeric’s effects, making this creamy, plant-based drink a powerful and delicious wellness boost to enjoy again and again.
Adjusting Your Lifestyle Habits Can Help Fatty Liver Disease
Nonalcoholic fatty liver disease is a silent but serious condition affecting millions worldwide. Its prevalence is closely tied to rising rates of obesity, type 2 diabetes, cardiovascular disease, and other lifestyle-related conditions. Management and prevention of these conditions and proactive lifestyle changes offer hope for preventing it and halting or even reversing its progression.
Tell us in the comments:
- Do you or someone you love have NAFLD?
- What lifestyle strategies will you adopt to prevent or manage NAFLD?
Featured Image: iStock.com/Prostock-Studio



