Your immune system plays a crucial role in protecting your body against harmful substances, germs, and even your cells. And if your immune system is weak, you’ll get ill often. So, it’s important to keep your immune system strong.
But sometimes “strong” isn’t enough (or may even be too much) — your immune system must also be smart. Autoimmune diseases occur when the immune system mistakenly attacks and damages healthy cells, tissues, and organs.
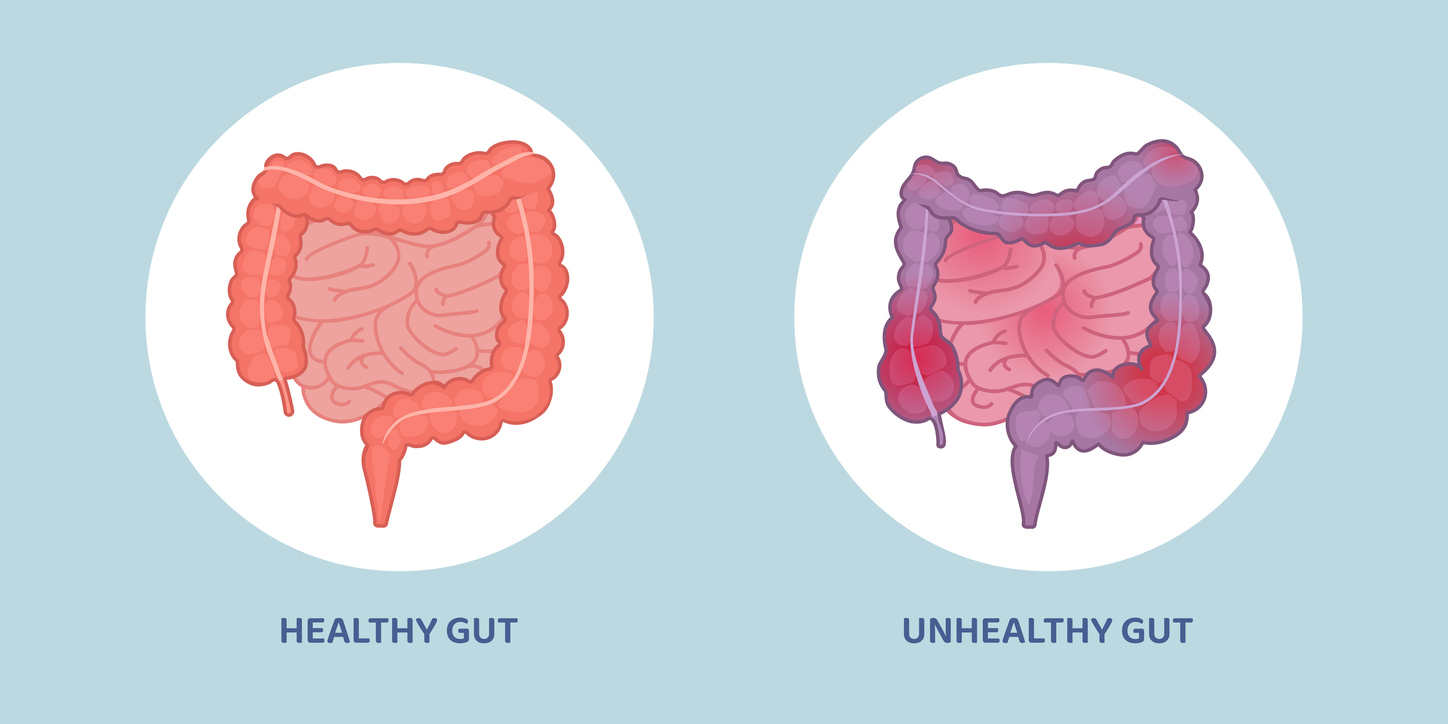
One of the areas sometimes attacked by a confused and overactive immune system is the digestive tract. When that happens, you can end up with conditions that fall under the umbrella of inflammatory bowel disease (IBD). The two most common IBD conditions are Crohn’s disease and ulcerative colitis. Between them, these two ailments are responsible for the vast majority of IBD cases.
Inflammatory bowel disease affects over two million Americans, and it’s estimated that more than seven million people in Europe and the US will suffer from IBD by 2030. And those are just the people who have been diagnosed. It’s estimated that the time to diagnosis can take 5–10 years in some cases. Some people may even have silent IBD where they are asymptomatic — or suffer from irritating symptoms without knowing why.
Public health professionals predict that as more people around the globe adopt Western dietary patterns and lifestyles, the prevalence of these diseases will continue to rise worldwide.
Which begs the question: what’s going on here? What factors are contributing to the rise in IBD and many other autoimmune diseases?
Recent research is pointing to lifestyle factors, especially diet, that may play a significant role in the development and progression of IBD. These factors may also be important in managing symptoms.
So, let’s explore these conditions, how they might occur, and what’s typically done to treat them. Then, we’ll look at how diet and gut health can be part of the problem or part of the solution.
IBD vs IBS
Before I describe them, I want to get a bit of alphabet soup out of the way. You may have heard of IBS, which stands for inflammatory bowel syndrome. IBS is similar to IBD, and the symptoms are often the same (bloating, diarrhea, constipation). However, the big difference is that IBS causes no inflammation and no lasting damage to the gastrointestinal (GI) tract.
Crohn’s disease and ulcerative colitis (the “IBD twins”), on the other hand, result from an immune system malfunction that causes it to attack healthy cells, leading to chronic inflammation and damage to the digestive tract.
Both diseases often develop in teenagers and young adults (frequently diagnosed before age 35), although the disease can occur at any age.
What Are Crohn’s Disease and Colitis?
Crohn’s disease and ulcerative colitis themselves are similar but distinct. There are three main differences.
First, Crohn’s disease can affect any part of the GI tract from mouth to anus (though it most commonly impacts the small intestine and colon). Ulcerative colitis, on the other hand, is limited to the large intestine (colon) and rectum.
Second, Crohn’s disease has healthy sections of the intestines and inflamed areas. In contrast, ulcerative colitis has continuous inflammation throughout the colon.
Third, inflammation manifests differently in each disease. Crohn’s often impacts multiple layers of the intestinal walls, while ulcerative colitis typically affects only the colon’s innermost lining.
Both conditions can cause symptoms like abdominal pain, cramping, fatigue, diarrhea, and weight loss. In more severe cases of either Crohn’s or colitis, chronic inflammation can damage the intestine, leading to complications like strictures (narrowings), fistulas (abnormal connections between the GI tract and other parts of the body, including the skin), and an increased risk of colon cancer.
Conventional Treatments for Crohn’s and Colitis

If you’re diagnosed with Crohn’s or colitis, you may be told there’s no cure and that the goal of any treatment will be to reduce inflammation, relieve symptoms, and prevent flare-ups and complications. As a result, treatment is usually drugs or surgery.
There are two classes of drugs used to treat IBD: anti-inflammatory drugs like corticosteroids (which can reduce symptoms) and immunosuppressive medications such as thiopurines and biologics, which can slow down the immune system’s onslaught on GI tract tissue.
Both drug classes can provide relief and aid with management but come with unpleasant and even dangerous side effects. While most of these unwanted effects typically stop when the steroid is stopped or the dose is lessened, a few, such as osteoporosis and cataracts, can persist and require treatment themselves.
Surgery is another option for IBD. For ulcerative colitis, surgery might mean removing part or all of the colon. This can relieve symptoms but also alters digestion in a major way. The most common surgery involves replacing the entire colon and rectum with a pouch that is connected to the anus. This allows the patient to have bowel movements in a somewhat more “normal” way.
Surgery for Crohn’s disease often involves removing damaged sections of the intestine. It’s not a permanent fix, as whatever caused the inflammation in the first place is liable to keep inflaming other areas.
In either case, surgery and drug treatments only treat the symptoms, not the cause. Because these approaches cannot alleviate the disease, many people look to complementary therapies, like dietary changes, to support their health — alongside or instead of traditional treatments. And as we’ll see a little later, these can be remarkably helpful.
What Causes IBD?

In general, scientists distinguish two categories of causes for any disease: genetic and environmental (which includes things like air, water, diet, and lifestyle). And there’s a clear genetic component to IBD. Certain populations are more prone to it than others (for example, in the US, there are higher rates of IBD among Caucasians than in the Hispanic and Black communities).
It also runs in families. A family history of IBD is often a predictor of whether someone will develop the disease. Of the two main types of IBD, Crohn’s disease appears to be more inheritable than ulcerative colitis.
You might think of genetics as the seeds of IBD. Like any seeds, they grow only under certain environmental conditions. A 2019 report on the results of 53 meta-analyses (does that make it a meta-meta-analysis?) identified nine environmental factors associated with an increased risk of IBD.
- Smoking
- Urban living
- Having undergone an appendectomy
- Having undergone a tonsillectomy
- Antibiotic exposure
- Oral contraceptive use
- Consumption of soft drinks
- Vitamin D deficiency
- Non-H pylori Helicobacter infection
The report also noted some environmental factors that protected against the development of IBD: being breastfed as an infant and engaging in physical activity. So, while you can’t redo your infancy without a time machine, you can start exercising now and take other critical steps to reduce your risk of developing inflammatory bowel disease.
The Importance of the Microbiome in IBD
In addition to genetic and environmental factors, there’s a third causal category in IBD: an imbalance in the gut microbiome. Each year, more evidence emerges about the connection between the health of your gut microbiome and GI tract inflammation. Both Crohn’s and colitis are characterized by gut microbiota dysbiosis, a decrease in the abundance and diversity of specific beneficial bacteria.
In particular, there’s a significant drop in Roseburia, Phascolarctobacterium, and Clostridium bacteria populations. These bacteria are big players in reducing inflammation in the digestive tract, largely through their production of short-chain fatty acids, or SCFAs.
SCFAs are crucial in fighting inflammation because they provide the energy to repair tissues within the gut. Without sufficient SCFAs, particularly, butyrate, your body can’t repair the damage caused by inflammation.
For more on SCFAs and how to help your microbiome make more of them, see our article here.
Your microbiome is also key to the functioning of your immune system. Much of your immune response originates in the gut, which holds between 70–80% of your body’s immune cells. When your microbiome is thrown off balance, immune cells can become overactive, leading to chronic inflammation and a misdirected attack on your body’s tissues.
The Role of Diet in Managing IBD
A growing body of research is showing us that the way you eat can make a big difference in whether IBD symptoms show up, how serious they are, and how frequently they occur.
Three diets with some research behind them are the specific carbohydrate diet, the low-FODMAP diet, and the plant-based diet.
The Specific Carbohydrate Diet

The specific carbohydrate diet (SCD) eliminates grains, sugars (except for honey), all milk products (except for hard cheeses and long-fermented yogurt), and most processed foods.
Although there aren’t many large-scale studies on SCD, A 2020 clinical trial of 18 young people (ages 7–18) with mild to moderate Crohn’s found that just 12 weeks on the diet helped relieve symptoms.
The Low-FODMAP Diet
The low-FODMAP diet is also used to treat IBS. It is so named because it aims to reduce the consumption of Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols (thank goodness for acronyms because that is a mouthful!).
These include fructans (found in garlic, onions, and some grains), fructose (from fruits, honey, and high-fructose corn syrup), galactans (beans and legumes), lactose (dairy products), and polyols (fruits with pits, such as apples, avocados, and cherries, and in sugar alcohols like sorbitol, xylitol, and mannitol.
While a diet low in FODMAPs can relieve symptoms and improve quality of life, it has one significant drawback: It eliminates some of the healthiest foods on the planet. Alliums (onions and garlic), legumes, and fruit are associated with stronger heart health, less cancer, better blood sugar control, and longevity.
Many people recommend starting on a low-FODMAP diet and slowly “graduating” to the diet with the most evidence in its favor for managing IBD: a whole foods, plant-based diet.
Plant-Based Diets and IBD

One reason whole foods, plant-based diets can help people with Crohn’s and colitis is what they leave out: meat and processed foods. Too much meat and processed foods can cause gut dysbiosis, promoting inflammation and withholding the energy needed to repair damaged digestive tissue.
However, whole foods, plant-based diets also contain lots of fiber, the favorite food of beneficial bacteria, especially those found in the colon. That’s one theory for why some people have achieved long-term remission of IBD symptoms while adhering to this way of eating.
A 2023 study found that a largely plant-based diet (which also included some yogurt and eggs) plus a drug, infliximab, used to treat autoimmune diseases was able to put 96% of the study participants in remission from Crohn’s. Even more significantly, over half of them remained symptom-free 10 years later. The researchers commented that the diet seemed to help patients tolerate and benefit from the infliximab, so the two treatments acted synergistically.
That said, listening to your body when you make dietary changes is important. Certain foods can either calm the digestive system or set off flare-ups, depending on individual triggers and the current state of the condition.
If you’re in a flare-up, you may need to avoid certain healthy foods, such as raw fruits and vegetables. Even if your body seems to react to these normally very healthy foods with a flare-up, you may be able to add these foods back gradually once the condition is in remission.
Anti-inflammatory and Gut-Supportive Foods for IBD

While many whole plant foods deliver fiber that nourishes your gut microbiome and helps fight inflammation, some foods are particularly good for that purpose. And as you’ll see, the list of foods that can be beneficial for IBD includes some truly delicious favorites.
One caveat before we jump in: all this research has two main shortcomings: the studies mostly included mice and rats, not humans, and they looked at extracts rather than whole foods. That said, there’s a good chance the results also apply to people and whole foods.
1. Purple Sweet Potatoes
Purple sweet potatoes are anti-inflammatory champs. A 2021 study found that an extract of anthocyanin, the antioxidant that gives the potatoes their rich purple hue, helped maintain gut health in mice with chronic colitis by balancing their gut microbiomes. And a 2024 study showed that the resistant starch in the sweet potatoes reduced the severity of colitis in mice. (Our view on the use of animals in medical research is here.)
To learn more about sweet potatoes, check out Are Sweet Potatoes Good for You? Everything You Need to Know.
2. Leafy Green Vegetables
A 2021 study examined a variety of foods and found that cooked leafy green vegetables, such as spinach and kale, were especially effective in reducing inflammation in people with Crohn’s disease in remission. This finding is especially meaningful because the study participants were humans, not rodents.
Get more tips on green veggies in Leafy Greens: How to Source, Wash, Store & Prepare Them.
3. Bananas
In 2024, researchers discovered that a protein we make after eating bananas, recombinant banana lectin, helped manage IBD in mice by enhancing their immune response. Green bananas may be even more effective, according to research. Another study found that combining green banana-resistant starch with a probiotic significantly reduced inflammation and improved gut health in mice with induced colitis.
For more on bananas, check out our article, Are Bananas Good for You?
4. Avocados
An ethanol extract from avocados was found to ease symptoms and reduce inflammation in mice with induced colitis by lowering levels of some inflammatory markers and blocking key inflammation pathways. Another study found that avocado seed oil reduced symptoms of ulcerative colitis in rats by lowering inflammation-related proteins, similar to the effects of sulfasalazine, a common medication used to treat the condition, but without side effects.
To find out more about avocados, check out Holy Guacamole! The Surprising Health Benefits of Avocados.
5. Nuts, Seeds, and their Butters
If you’re a fan of nuts, seeds, and their butters, you might be happy to hear that compounds found in these foods can also help fight IBD. Several case studies of people who went into complete remission of symptoms show that daily consumption of peanut butter, pumpkin seeds, flaxseeds, and hemp seeds was associated with symptom improvement.
Find more surprising facts about nuts in Nut Health Benefits: You Won’t Believe How Good They Are for You.
6. Fermented Foods
Fermented foods can help by increasing populations of beneficial bacteria. A study of the rising incidence of IBD in Japan blames it on the fact that modern Japanese people are eating less fermented food than in the past.
For more on the benefits of good gut bacteria foods, check out our article on Fermented Foods: What are they and how can they boost your health?
7. Green Tea
Green tea, also deserving of a spot in the anti-IBD Hall of Fame, contains polyphenols that have been found to reduce inflammatory compounds and boost protective antioxidant activity.
Discover more benefits of green tea in the 5 Science-Backed Reasons to Drink Matcha Tea.
Foods and Ingredients to Limit or Avoid With IBD

While we’re just beginning to explore how whole plant foods can prevent and treat IBD, we have more evidence showing that certain other foods can promote irritable bowel disease.
1. Red and Processed Meat
A 2022 study investigated the relationship between protein intake and the risk of IBD in over 413,000 people. Over a 16-year follow-up, the study found that while total protein (animal or vegetable) intake was not associated with Crohn’s disease or ulcerative colitis risks, higher consumption of meat — particularly red meat — was linked to an increased risk of ulcerative colitis. These findings suggest that reducing meat consumption may benefit individuals at high risk of developing certain types of IBD.
2. Sugar-Sweetened Beverages
Too much sugar is detrimental to a lot of health conditions, and there’s an interesting link between sugar consumption and Crohn’s and colitis.
A 2023 study looked at how drinking sugar-sweetened beverages, like soda and juices, affects people with IBD conditions. The study followed over 1,100 patients for up to three years, and researchers found that drinking a lot of sweet beverages (seven or more per week) was linked to higher levels of inflammation and worse disease symptoms. These patients also ended up in the hospital or emergency room sooner than those who drank fewer sugary drinks. The findings were confirmed in another group of patients, suggesting that cutting back on sugary drinks might help people with IBD manage their condition better.
3. Alcohol
A recent review explored how alcohol consumption affects people with IBD. Drinking alcohol is linked to a higher risk of symptom flare-ups and worse GI symptoms. Alcohol can interfere with medications used to treat IBD, potentially making them less effective or increasing side effects.
Read more about alcohol and your health in Alcohol: Its Effects, Risks, Uses & Potential Benefits.
4. Processed Foods
A recent study explored how processed foods and food additives might influence the development of Crohn’s disease in different regions. Researchers compared the diets of 274 Crohn’s patients with those of their relatives, household members, and unrelated healthy controls. They found that Crohn’s patients consumed more processed foods during early life, especially soft drinks, fast food, and processed snacks. This pattern is held across regions, with patients in Hong Kong and China showing especially high additive consumption. These findings suggest that early and ongoing exposure to processed foods and additives may contribute to Crohn’s disease development and persistent inflammation.
Find out more about the dangers of processed foods in The Sad Diet: Ultra-Processed Foods and Their Impact on Depression.
5. Sweets
A 2021 review summarized findings from studies examining how dietary carbohydrates, sugar, and sugar-sweetened beverages affect the risk of IBD. The researchers found no correlation between overall carbohydrate consumption and IBD risk. However, they found that consuming carbohydrates from sugar was linked to a greater risk of developing both Crohn’s disease and ulcerative colitis. These findings suggest that reducing sugar consumption might help lower the likelihood of developing IBD.

Nutritional Deficiencies and Supplementation for IBD
Dietary strategies for dealing with IBD aren’t just about mitigating symptoms or reversing disease progression. You also have to pay attention to getting enough of the nutrients humans need to be healthy because chronic inflammation and the body’s impaired ability to absorb nutrients during flare-ups can lead to nutrient deficiencies.
Common deficiencies among people with IBD include iron, vitamin D, calcium, and vitamin B12.
Iron deficiency can occur due to intestinal bleeding and reduced consumption of iron-containing foods — either due to dietary preference or symptom flare-ups from foods like legumes.
Vitamin D and calcium are critical nutrients as they support bone health, which can be compromised by the long-term use of the corticosteroid medications commonly prescribed for IBD.
B12 deficiencies are also common in people with Crohn’s. That’s true, especially after surgery, to remove parts of the small intestine since that’s where B12 is primarily absorbed. In these cases, B12 injections or sublingual supplements may be recommended.
To find out more about these nutrients, where to get them, and how much you need, check out these in-depth articles:
- The Truth About Iron + Why Plant-Based Foods Are the Best Way to Get the Iron You Need
- Vitamin D Guidelines: What Is It, How Much Do You Need & How to Get Enough
- The Healthiest Way to Get the Calcium You Need + 9 Calcium-Rich Foods
- Vitamin B12: Why it’s Important and How to Avoid B12 Deficiency
If you’re living with IBD, regular blood testing is highly recommended to ensure you’re getting enough of these and other critical nutrients.
Supplements may sometimes be required to keep your levels in the normal range. They can certainly help bridge the gap, but they should be used carefully and probably under the supervision of a healthcare provider to avoid digestive discomfort or interactions with medications.
So, the bottom line is that there’s hope. By eating certain foods and steering clear of others, incorporating certain key supplements, and taking helpful lifestyle approaches, many people with IBD can better manage deficiencies and potentially even put the condition into remission.
Recipes for Crohn’s and Colitis
These three plant-based recipes are packed with gut-loving ingredients and are great for most people managing IBD. They’re rich in fiber, anti-inflammatory goodness, and various plants to help keep your gut happy. Easy, delicious, and nourishing, these dishes make caring for your digestion fun and flavorful!
1. Kimchi Avocado Toast

Kimchi Avocado Toast is a tasty, gut-friendly breakfast that can be especially beneficial for those managing Crohn’s or colitis. Creamy avocado provides healthy fats that are easy on digestion, while probiotic-rich kimchi helps balance gut bacteria. Fresh, crunchy veggies like cucumber and radish add extra nutrients, and a squeeze of lime brightens the flavors. Packed with fiber, prebiotics, and probiotics, this toast is a deliciously simple way to nourish and support a healthy gut.
2. Purple-Powered Lunch Bowl With Crispy Chickpeas

The Purple-Powered Lunch Bowl With Crispy Chickpeas is a flavorful, gut-friendly choice, especially beneficial for those managing IBD. Purple potatoes, beets, and red cabbage are rich in anthocyanins, natural compounds that help reduce gut inflammation and promote overall gut health. A drizzle of our Tangy Blueberry Dressing adds a fresh berry flavor and extra anti-inflammatory benefits. With crispy chickpeas, vibrant veggies, and fresh greens, this bowl is both satisfying and deeply nourishing.
3. Green Tea Pistachio Nice Cream

Green Tea Pistachio Nice Cream is a creamy, wholesome treat that’s delicious and nourishing. Made with ripe bananas, coconut cream, and a touch of matcha powder, it’s a sugar-free dessert packed with antioxidants that can help reduce inflammation — especially great for those with IBD. Pistachios add a crunchy, nutty twist that perfectly complements the smooth texture. This simple, flavorful dessert is a delightful way to satisfy your sweet tooth while caring for your gut health!
There Is Hope with Crohn’s and Colitis
Crohn’s disease and ulcerative colitis are autoimmune conditions that cause chronic inflammation in the digestive tract, leading to symptoms that can disrupt daily life. While there’s no known cure, a combination of medical treatments and lifestyle adjustments can help manage these challenging conditions.
A plant-based diet, in particular, can be a powerful tool in managing IBD. Avoiding personal trigger foods (especially during a flare-up) and those generally not recommended can help manage quality of life. In addition to incorporating nutrient-dense foods, supplementation may be necessary in some cases because of problems with nutrient absorption.
Living with Crohn’s and colitis is a journey that involves trial and error. Finding the right blend of medical interventions and dietary choices can help improve health and well-being.
Tell us in the comments:
- Are you or someone you love dealing with IBD?
- What foods or types of diets have helped reduce or eliminate your symptoms?
Featured Image: iStock.com/Panuwat Dangsungnoen



